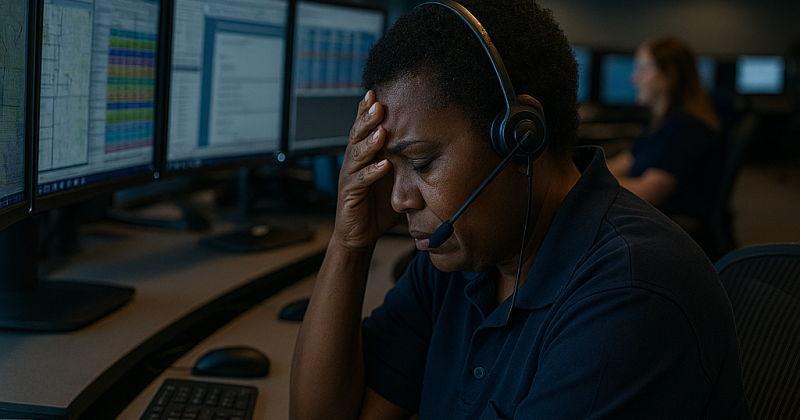
Post-traumatic stress disorder (PTSD) is often associated with first responders on the front lines—Firefighters, EMS crews, and law enforcement officers. But what’s often forgotten is that Dispatchers are exposed to trauma, too—just from a different angle. You hear the screams. You walk people through the worst moments of their lives. You send help but stay behind. Over time, that emotional weight adds up, often in silence.
For too long, PTSD among Dispatchers has been underrecognized, misdiagnosed, or dismissed as “just stress.” But this job changes people. And when those changes affect sleep, relationships, emotional health, or job performance, it’s time to pay attention. This article outlines the signs of dispatcher PTSD and how to get the help you deserve.
Recognizing the Signs of PTSD in Dispatchers
📌 Common Symptoms
- Intrusive memories or flashbacks of specific calls
- Avoidance of certain types of calls (e.g., pediatric, suicide)
- Increased irritability or anger
- Emotional numbness or detachment
- Hypervigilance (constantly feeling “on edge”)
- Difficulty sleeping or recurring nightmares
- Guilt or shame over perceived failures, even when unwarranted
📌 Behavioral Clues in the Center
- Withdrawing from coworkers or isolating
- Overcompensating with work perfectionism
- Increased absenteeism or frequent sick leave
- Risky behavior outside of work (alcohol, reckless driving, etc.)
Real-World Example: Wendy Bundy’s Story
Wendy Bundy, a former 911 dispatcher, has openly shared her personal journey with PTSD. In a candid interview, she recounted how the cumulative stress from handling traumatic calls—such as guiding a caller through CPR on a dying child—led to severe anxiety, nightmares, and emotional numbness. Despite the invisible nature of her wounds, the psychological toll was profound, affecting both her professional performance and personal relationships. Wendy’s experience highlights the often-overlooked mental health challenges faced by emergency dispatchers and underscores the importance of acknowledging and addressing these issues within the profession.
Why PTSD Hits Dispatchers Differently
No closure:
Dispatchers rarely know the outcome of the calls they handle.
Chronic exposure:
Unlike field responders who may have recovery time, Dispatchers jump from one traumatic call to the next—often in a single shift.
Emotional conflict:
Helping people through trauma without physically intervening can lead to a sense of helplessness.
Cultural silence:
Historically, Dispatcher wellness wasn’t discussed—asking for help was seen as weakness.
When It’s More Than Stress: Knowing When to Seek Help
🚨 Red Flags That Warrant Professional Support:
- Suicidal thoughts or self-harm ideation
- Panic attacks or intense fear reactions during calls
- Inability to function at home or work
- Substance dependence to “numb” feelings
🛠️ First Steps to Take:
Talk to someone:
Peer support teams or trusted supervisors can help begin the conversation.
Find a specialist:
Look for a mental health provider trained in trauma, ideally one familiar with first responders or dispatch work.
Explore EAP options:
Many agencies offer free counseling through Employee Assistance Programs.
Practice grounding:
Learn basic coping skills such as box breathing or 5-4-3-2-1 sensory grounding to manage panic and anxiety.
Internal Resources from The Alarm Room
- Building Resilience: Training Dispatchers to Handle Traumatic Calls
- Crisis Within the Crisis: Supporting a Teammate Through Mental Health Struggles
Conclusion
Being a Dispatcher means living in a world where stress is expected—but trauma shouldn’t be normalized. PTSD is not a sign of weakness. It’s a sign that your brain is reacting to relentless exposure to emergencies. And help is not only available—it’s necessary.
You’ve helped countless people. Now it’s time to help yourself or your teammates. If something in this article resonated with you, please consider sharing it with your team, commenting with your thoughts, or subscribing to receive more mental health resources directly to your inbox.